You know the pressure of a packed waiting room. Patients need answers fast, the phone won't stop ringing, and one missing test result can throw an entire day off balance.
Over the last decade, technology in healthcare has moved far beyond basic scheduling tools. Today, specialized systems help track every patient detail, streamline communication between departments, and keep life-saving decisions from getting stuck in delays.
Here are five types of software that have become the backbone of modern healthcare.
Quick Answer: What Are the Main Types of Software Used in Healthcare?
The five essential types of software transforming healthcare delivery are:
- Electronic Health Records (EHR) systems that centralize patient data, medical histories, and clinical documentation in one accessible location.
- Practice Management Software that handles scheduling, billing, insurance verification, and administrative workflows.
- Telemedicine Platforms enabling remote consultations, virtual care delivery, and patient monitoring from home.
- Medical Imaging and Diagnostic Software for capturing, analyzing, and sharing X-rays, MRIs, CT scans, and other diagnostic images.
- Healthcare Analytics Platforms that transform raw clinical and operational data into actionable insights for improving outcomes and reducing costs.
These systems work together to improve patient outcomes, reduce operational costs, and streamline care delivery across hospitals, clinics, and healthcare organizations of all sizes. Understanding each type helps you identify gaps in your current technology stack and prioritize investments that deliver the greatest clinical and financial impact.
Key Takeaways
- The five essential types of healthcare software are EHR systems, practice management software, telemedicine platforms, medical imaging software, and healthcare analytics platforms. Each serves a distinct purpose, but they work best when integrated to create a seamless healthcare ecosystem.
- Electronic Health Records (EHR) systems form the digital backbone of modern healthcare, centralizing patient information and enabling coordinated care across departments and facilities while ensuring data follows patients wherever they receive treatment.
- Practice management software streamlines administrative operations, reducing overhead costs by up to 30% while improving patient satisfaction through efficient scheduling, automated billing, and intelligent no-show prediction.
- Telemedicine platforms have become essential infrastructure, expanding access to care and creating new revenue streams for healthcare providers through AI-powered consultations, remote monitoring, and accessible virtual care options.
- Medical imaging and diagnostic software enhance clinical accuracy, enabling faster diagnoses and better treatment planning through advanced visualization tools, with AI-assisted systems achieving up to 94% diagnostic accuracy in detecting lung nodules.
- Healthcare analytics platforms transform raw data into actionable insights, helping organizations improve outcomes while reducing costs in areas where custom healthcare solutions excel at delivering measurable ROI and competitive advantage.
Understanding the Healthcare Software Ecosystem
Walk into any hospital today, and you'll see how much has changed. Tablets have replaced clipboards, lab results reach doctors in seconds, and scheduling runs smoother than it used to.
None of this happens on its own. It's the software behind the scenes making sure every part of patient care stays connected.
The shift isn't small. Healthcare IT is now a $360 billion market in 2024 and is on track to grow past $730 billion by 2029. The biggest jumps are coming from tools changing how care is delivered every day:
- Telemedicine platforms are expected to pass $115 billion this year, making remote care standard in many practices.
- AI-driven diagnostics, already a $9+ billion market, are helping doctors make faster, safer calls on treatment.
- Cloud-based data storage, worth over $40 billion, keeps records accessible without sacrificing security.
Yet, most hospitals don't run on a single platform. A patient might book online through one system, have vitals entered in another, receive results elsewhere, and handle billing on yet another.
When those systems don't talk to each other, mistakes and delays follow. Building a connected setup isn't just a "tech upgrade"; it's what keeps care moving without the daily chaos.
Why Healthcare Organizations Need Multiple Software Types
Healthcare delivery isn’t a single process. It’s a complex web of interconnected workflows happening all at once. A single patient visit can set off a chain of actions across scheduling, clinical documentation, lab orders, imaging, billing, and follow-up care. No single software can manage all of that effectively.
That’s why modern healthcare organizations rely on a connected ecosystem of specialized tools. Each system focuses on doing one job exceptionally well, but the real impact comes when these tools work together.
For example, when your EHR integrates with practice management software, patient data moves seamlessly from check-in to billing without redundant data entry. And when telemedicine platforms connect with analytics systems, providers can identify care gaps early and take proactive action before issues escalate.
Organizations don’t fail because they have too many systems. They fail because those systems don’t talk to each other, forcing staff to manually move data between platforms, creating inefficiencies, and increasing the risk of costly errors.
Healthcare Software Interoperability Challenges
Integration sounds easy on paper, but in practice, it’s one of healthcare IT’s biggest challenges. Different vendors follow different data standards, legacy systems resist sharing information, and every integration must meet stringent security requirements.
Industry standards like HL7 and FHIR were developed to solve this, but adoption remains inconsistent. Some vendors embrace open APIs and smooth integrations, while others lock data behind proprietary formats that require expensive custom workarounds.
If you’re evaluating new healthcare software, interoperability is non-negotiable. Before signing any contract, ask vendors:
- What APIs and data exchange options do you provide?
- Can your platform export data in standardized formats?
- Do you integrate with our current EHR or lab systems?
Fixing integration issues later often costs far more than investing in the right system upfront.
And beyond technical compatibility, there’s compliance to consider. HIPAA sets strict rules on how patient data is accessed and transmitted. HITRUST certification adds another layer of assurance for security management across connected systems. For software that touches medical devices or diagnostics, FDA regulations also apply.
In short, the right healthcare software isn’t just about functionality. It’s about seamless interoperability, robust security, and guaranteed compliance from day one.
5 Different Types of Software Used in the Healthcare Industry
1. Electronic Health Records (EHR) Systems
Every patient interaction creates data: a diagnosis, a prescription, a test result, a follow-up plan. Without an organized system, that information gets scattered, lost in paper files, or siloed in separate departments.
EHR systems solve this problem by becoming the central hub for all patient information within a hospital or clinic.
Their value isn't just theoretical. In a large-scale survey assessing the usefulness of EHRs, healthcare professionals reported:
- 93.7% agreed EHRs cut costs by reducing paperwork, improving safety, avoiding duplicate tests, and streamlining care.
- 93.1% said they improved document legibility, reducing errors caused by unclear handwriting or misplaced files.
- 92.7% found they made secure information sharing easier, helping clinicians and patients stay on the same page.
- 92.7% highlighted simplified coding and documentation, easing the administrative load.
But the real power of EHRs goes beyond storing information. Modern platforms act as connectors across the healthcare ecosystem.
They exchange data seamlessly with laboratories, pharmacies, imaging centers, and other providers using standardized protocols like HL7 and FHIR. This interoperability ensures a patient's information follows them wherever they go, reducing duplicate testing, preventing gaps in care, and improving coordination between teams.
Choosing the right EHR is a long-term decision with a direct impact on efficiency and patient safety. Off-the-shelf solutions don't always fit unique workflows, which is why many organizations invest in custom healthcare software development. Tailored systems can improve usability for staff, support compliance with strict regulatory standards, and evolve as new technologies and care models emerge.
Key Features of Electronic Health Records Systems
Modern EHR systems include:
- Clinical documentation tools with templates, voice recognition, and smart phrases to speed up charting
- Computerized physician order entry (CPOE) that reduces medication errors and automates order routing
- Clinical decision support that alerts providers to drug interactions, allergies, and guideline-based care recommendations
- Patient portals that give patients 24/7 access to their records, test results, and secure messaging with providers
- Population health management tools that identify care gaps and at-risk patients across patient panels
- Reporting and analytics for quality measures, meaningful use attestation, and operational metrics
Best Use Cases for EHR Systems in Healthcare
EHRs deliver the most value when:
- Coordinating complex care across multiple specialists. A patient with diabetes, heart disease, and kidney problems sees multiple providers. The EHR ensures everyone has the complete picture, reducing dangerous gaps in coordination.
- Supporting value-based care models. ACOs and bundled payment programs require tracking quality metrics across populations. EHRs provide the data infrastructure to monitor performance and identify improvement opportunities.
- Improving medication safety. Electronic prescribing with clinical decision support catches potential problems before they reach the patient. Allergy alerts, dose checking, and formulary information reduce adverse drug events significantly.
Integration Points with Other Healthcare Software Types
EHRs serve as the central hub, connecting to:
- Practice management software for seamless patient registration, appointment scheduling, and demographic data sharing
- Telemedicine platforms to incorporate virtual visits into the patient's longitudinal record
- Medical imaging systems to display radiology results alongside clinical notes
- Healthcare analytics platforms to feed clinical data for population health analysis and quality reporting
2. Practice Management Software
Delivering great care doesn't just depend on clinical expertise. It also depends on how well the practice is managed behind the scenes.
From booking appointments to handling insurance claims, a smooth administrative process keeps the entire operation running efficiently. That's where practice management software comes in.
At its core, this software manages day-to-day operational tasks, but modern platforms do much more than basic scheduling:
- Smarter Scheduling: Advanced systems optimize appointment slots based on provider availability, procedure length, and patient preferences. Many now predict the likelihood of no-shows and automatically fill gaps from a waitlist, helping practices avoid wasted time. In fact, intelligent reminders and automated waitlist management can reduce no-show rates by up to 30%, directly protecting revenue streams.
- Streamlined Financial Processes: These platforms verify insurance eligibility in real time, submit claims electronically, flag potential errors before submission, and manage denials. Automation here cuts administrative workload and accelerates the revenue cycle, meaning providers get paid faster.
- Data-Driven Decision-Making: Built-in reporting tools let managers track financial performance, spot inefficiencies, and identify opportunities to increase productivity and profitability.
Integration is where practice management software delivers its biggest payoff. When it's connected to the EHR, patient information flows automatically between systems. This means no duplicate data entry, fewer errors, and less time spent juggling platforms. Staff can focus on patients instead of paperwork, while the software handles the heavy lifting of scheduling and billing in the background.
Key Features of Practice Management Software
Core capabilities include:
- Multi-location scheduling with provider calendars, room management, and recurring appointment templates
- Patient registration and demographics with insurance verification and eligibility checking
- Charge capture and claims management with electronic submission, scrubbing tools, and denial tracking
- Payment processing supporting co-pays, patient balances, payment plans, and credit card processing
- Reporting dashboards showing collections, accounts receivable aging, provider productivity, and appointment statistics
- Patient communication tools including automated reminders, recall systems, and broadcast messaging
Best Use Cases for Practice Management Software in Healthcare
Practice management software excels at:
- Maximizing provider productivity. By optimizing schedules and reducing administrative time, physicians can see more patients without working longer hours. Automated tasks like insurance verification happen in the background instead of consuming front-desk time.
- Improving revenue cycle performance. Clean claims submission, proactive denial management, and patient balance tracking accelerate collections and reduce write-offs. Practices typically see 5-10% improvements in overall collections within the first year.
- Enhancing patient experience. Online scheduling, automated reminders, and transparent billing reduce friction points. Patients appreciate the convenience, and practices benefit from reduced no-shows and faster payments.
Integration Points with Other Healthcare Software Types
Practice management systems connect to:
- EHR systems for bi-directional patient demographic sharing and appointment-based documentation
- Healthcare analytics platforms to analyze operational efficiency, financial performance, and patient satisfaction metrics
- Telemedicine platforms to schedule virtual visits and capture revenue from remote care delivery
- Medical imaging systems for scheduling and tracking imaging orders and results
3. Telemedicine Platforms
Telemedicine has evolved from a stopgap solution into an essential part of modern healthcare. Providers can now deliver real-time, high-quality care beyond the walls of a clinic, supported by tools that make virtual visits faster, more accurate, and more accessible to patients everywhere.
Modern platforms go beyond secure video calls. They combine AI-driven intelligence, real-time diagnostics, and connected health monitoring to create a truly comprehensive virtual care environment:
- AI-powered Consultations: Multimodal AI analyzes patients' speech, facial cues, and medical history during visits, assisting with diagnosis and treatment planning. AI scribes automatically document the consultation, cutting manual note-taking time by up to 72%.
- Accessible Virtual Care: Progressive Web Apps allow telemedicine to function on low-speed connections, expanding access for rural communities. Real-time AI translation and text-to-speech features make care available to non-native speakers and patients with disabilities.
- Continuous Health Monitoring: Integration with wearables and IoT devices streams real-time vitals and long-term health data directly to providers. Predictive analytics dashboards flag early warning signs, allowing timely interventions before conditions escalate.
- Streamlined Workflows: AI-guided symptom checkers collect patient information upfront, reducing intake time. Automated scheduling, billing, and EHR updates keep records accurate and complete without extra administrative work.
- Extended Specialist Reach: Remote-controlled robotic assistance allows specialists to consult or even perform certain procedures for patients in remote or underserved locations.
Behind the scenes, robust infrastructure ensures reliability and security. Telemedicine platforms use secure data transmission protocols to protect patient privacy and maintain HIPAA compliance.
Automated documentation features feed directly into the EHR, ensuring continuity of care and reducing the risk of missing information. Queue management tools help providers handle high volumes of virtual appointments efficiently, cutting wait times and improving the patient experience.
For organizations planning to scale their telemedicine capabilities, many start with a minimum viable platform (MVP). This approach allows providers to test workflows, gather real-world feedback from patients and clinicians, and refine the system before committing to a full-scale rollout.
A well-designed MVP helps avoid costly implementation mistakes and ensures the platform truly fits the needs of both patients and staff.
Key Features of Telemedicine Platforms
Essential telemedicine capabilities include:
- Secure HD video conferencing with HIPAA-compliant encryption and reliable performance on varying bandwidth
- Virtual waiting rooms with queue management and automated patient intake workflows
- Screen sharing and annotation tools for reviewing test results, images, and educational materials during visits
- E-prescribing integration allowing providers to send prescriptions directly from the telehealth encounter
- Remote monitoring device integration connecting blood pressure cuffs, glucometers, pulse oximeters, and other home health devices
- Asynchronous messaging and store-and-forward capabilities for non-urgent consultations and follow-up communication
Best Use Cases for Telemedicine Platforms in Healthcare
Telemedicine delivers maximum impact for:
- Expanding access in rural and underserved areas. Patients who previously traveled hours for specialist consultations can now connect virtually. This is convenient and life-changing for communities lacking local specialty care.
- Managing chronic conditions remotely. Regular check-ins via telemedicine, combined with remote monitoring data, help providers catch problems early. Patients with diabetes, heart failure, or COPD benefit from more frequent touchpoints without the burden of traveling to appointments.
- Providing behavioral health services. Telepsychiatry and virtual counseling reduce barriers to mental health care. Patients feel more comfortable receiving therapy from home, and providers can reach more patients by eliminating geographic constraints.
Integration Points with Other Healthcare Software Types
Telemedicine platforms integrate with:
- EHR systems to automatically document virtual visits, capture billing codes, and maintain complete patient records
- Practice management software for seamless scheduling of both in-person and virtual appointments
- Medical imaging systems for real-time review of radiology studies during remote consultations
- Healthcare analytics platforms to track telehealth utilization, patient outcomes, and quality metrics across virtual care programs
4. Medical Imaging and Diagnostic Software
Medical imaging and diagnostic software has completely changed how clinicians interpret and act on patient data. Instead of relying on film-based systems, today's applications process, store, and visualize images from X-rays, MRIs, CT scans, and ultrasounds with remarkable speed and precision. These tools help doctors detect diseases earlier, diagnose with greater confidence, and plan treatments more effectively.
At the core of most hospitals' imaging infrastructure is the Picture Archiving and Communication System (PACS). PACS solutions centralize image storage and allow authorized providers to access scans securely from anywhere, improving collaboration between specialists.
Many of these platforms now use AI algorithms that can detect abnormalities, measure anatomical structures, and even predict disease progression by analyzing subtle imaging patterns that might be missed by the human eye.
Integration is another critical factor. When imaging software links directly to a patient's electronic health record (EHR), radiologists and physicians can instantly compare new images with historical ones, review relevant medical notes, and make faster, better-informed decisions. This connectivity reduces delays in diagnosis, prevents unnecessary repeat imaging, and ensures every specialist involved in a patient's care has the same complete picture.
Real-world use cases highlight the transformative potential of these tools. A collaboration between Massachusetts General Hospital (MGH) and the Massachusetts Institute of Technology (MIT) developed an AI-powered diagnostic solution for radiology, trained on large datasets of annotated medical images.
The results were striking:
- 94% diagnostic accuracy in detecting lung nodules on X-rays and CT scans, compared to approximately 65% accuracy among human radiologists in similar cases.
- AI-assisted workflows relieved radiologists from repetitive analysis tasks, giving them more time to focus on complex cases and reducing burnout.
- Faster and more reliable diagnoses accelerated treatment initiation, directly improving patient outcomes.
Additionally, AI-driven predictive analytics integrated with diagnostic imaging is being employed at Johns Hopkins Hospital in collaboration with Microsoft Azure AI. The AI models analyze patient data from imaging, EHRs, and genomics to predict disease progression and readmission risks, enabling earlier interventions and more personalized care.
These case studies illustrate where medical imaging software is heading: AI-enhanced diagnostic tools that boost accuracy, speed, and efficiency across healthcare systems worldwide.
Key Features of Medical Imaging and Diagnostic Software
Core imaging software capabilities include:
- DICOM-compliant image storage and retrieval supporting all major imaging modalities (X-ray, CT, MRI, ultrasound, PET)
- Advanced visualization tools including 3D reconstruction, multi-planar reformatting, and fusion imaging
- Worklist management and reporting tools that streamline radiologist workflows and automate report distribution
- AI-powered detection and measurement for lung nodules, fractures, hemorrhages, and other critical findings
- Vendor-neutral archives (VNA) that consolidate imaging data across multiple PACS instances
- Structured reporting templates using RadLex and other standardized terminologies
Best Use Cases for Medical Imaging and Diagnostic Software in Healthcare
Medical imaging software excels at:
- Emergency radiology triage. AI algorithms flag critical findings like intracranial hemorrhage or pneumothorax, alerting radiologists and clinicians immediately. This automation can save minutes or hours in time-critical situations where delays cost lives.
- Chronic disease monitoring. Serial imaging comparison tools track disease progression in cancer patients, monitor aneurysm growth, or assess treatment response. Automated measurements ensure consistency across time points and different readers.
- Subspecialty collaboration. Cloud-based PACS enables remote consultations with subspecialists. A rural hospital can have a neuroradiologist review a complex brain MRI within minutes, improving diagnostic confidence without patient transfer.
Integration Points with Other Healthcare Software Types
Medical imaging systems connect to:
- EHR systems to embed imaging results in patient charts and link studies to clinical context
- Practice management software for scheduling imaging procedures and tracking orders from request through completion
- Telemedicine platforms to enable remote image review during virtual consultations
- Healthcare analytics platforms to analyze imaging utilization, turnaround times, and quality metrics
5. Healthcare Analytics and Business Intelligence Platforms
Modern healthcare produces more data than ever before, from patient records and lab results to insurance claims and operational metrics. In fact, global healthcare data storage is expected to reach 175 zettabytes by 2025.
The challenge isn't collecting this information. It's turning it into insights that actually improve patient care and organizational performance.
That's where healthcare analytics and business intelligence (BI) platforms come in. These tools connect data from multiple sources, clean it, and transform it into clear, actionable dashboards for decision-makers across hospitals and clinics.
The impact spans three major areas:
- Population Health Management: Predictive models flag high-risk patients before serious complications develop. This proactive approach helps providers intervene early, reducing avoidable hospitalizations and improving long-term outcomes.
- Operational Efficiency: Analytics platforms spot trends in patient flow, staff workloads, and equipment usage. Hospitals using real-time dashboards have reported up to a 15% boost in bed utilization, reducing wait times and making better use of limited resources.
- Financial Performance: BI tools highlight patterns in denied claims and payment delays. Some providers have seen 5–10% improvements in collections by using analytics to refine billing processes and revenue cycle management.
Real-world results highlight just how powerful these platforms can be. University of Pittsburgh Medical Center (UPMC) aggregated data from electronic health records, insurance claims, and patient surveys using its BI platform.
By identifying at-risk patients and planning targeted interventions, UPMC cut hospital readmissions by 30% and improved chronic disease management outcomes by 20%.
As data volumes continue to surge, the healthcare organizations that thrive won't just be those with the most data; they'll be the ones that can interpret and act on it effectively, using BI platforms to bridge the gap between information and better patient care.
Key Features of Healthcare Analytics Platforms
Advanced analytics platforms provide:
- Real-time operational dashboards tracking ED wait times, bed availability, surgical schedules, and staff productivity
- Clinical quality reporting measuring HEDIS, MIPS, and other quality metrics with automated data collection
- Financial analytics monitoring revenue cycle KPIs, payer mix, denial rates, and cost per case
- Population health risk stratification identifying patients most likely to benefit from care management programs
- Predictive modeling capabilities forecasting readmission risk, no-show probability, and disease progression
- Natural language processing (NLP) extracting insights from unstructured clinical notes and documentation
Best Use Cases for Healthcare Analytics Platforms in Healthcare
Analytics platforms deliver value through:
- Value-based care program management. ACOs and bundled payment participants need detailed performance tracking across attributed populations. Analytics platforms measure quality gaps, identify high-cost outliers, and quantify savings opportunities.
- Revenue cycle optimization. Denial patterns, payer performance, and collection rates become visible through financial analytics. Organizations can target improvement efforts where they'll have the biggest financial impact.
- Clinical variation reduction. Physician performance dashboards highlight practice pattern differences in cost and quality metrics. When providers see their results compared to peers, they naturally move toward evidence-based best practices.
Healthcare analytics platforms aggregate data from:
- EHR systems for clinical data, quality measures, and patient outcomes
- Practice management software for financial data, scheduling patterns, and operational metrics
- Telemedicine platforms to track virtual care utilization and outcomes
- Medical imaging systems for radiology turnaround times, study volumes, and critical finding response metrics
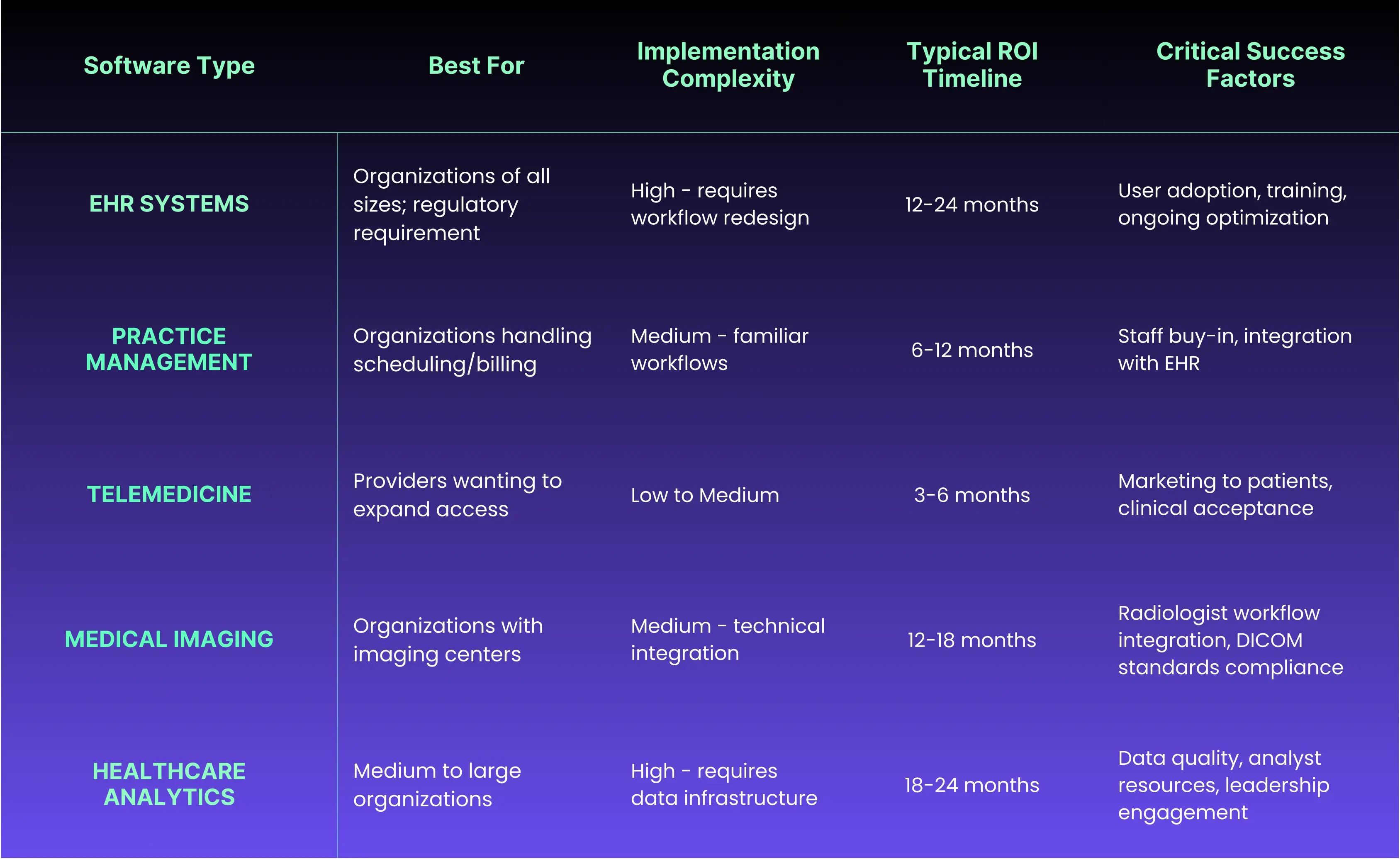
Which One Does Your Organization Need?
Not all organizations need all five software types immediately. Your priorities depend on size, specialty, current pain points, and strategic goals. Here's how to think about sequencing and prioritization.
Small Practices (1-10 Providers)
- Start With: Practice management software and EHR combined in an integrated platform. Small practices can't afford separate systems that don't talk to each other. All-in-one solutions from vendors like Epic, eClinicalWorks, or Athenahealth minimize integration headaches.
- Add Next: Telemedicine capabilities. Virtual visits became table stakes during COVID and aren't going away. Look for telemedicine built into your EHR rather than standalone platforms.
- Defer: Advanced analytics and business intelligence. You don't have the data volume to make sophisticated analytics worthwhile yet. Focus on core operations first.
Medium Practices (11-50 Providers)
- Start With: Upgrading to best-of-breed systems if currently using an all-in-one platform. At this scale, specialized tools often outperform generalist platforms. Consider separate but integrated EHR, practice management, and billing systems.
- Add Next: Healthcare analytics for population health management. You now have enough patients to benefit from risk stratification and care gap identification. Analytics pay for themselves through value-based care incentives.
- Consider: Advanced medical imaging software if operating imaging centers. PACS becomes cost-effective when you're processing hundreds of studies monthly.
Large Healthcare Systems (50+ Providers)
- Must Have: Enterprise EHR with robust interoperability, comprehensive analytics platform, and advanced practice management capabilities. At this scale, integration and data governance become critical.
- Strategic Priority: Telemedicine infrastructure and remote monitoring programs. Large systems can justify the investment in platforms that support multiple service lines and specialties.
- Competitive Advantage: AI-powered diagnostic software and predictive analytics. Early adopters of advanced technology gain quality and efficiency advantages that differentiate them from competitors.
Choosing the Right Healthcare Software Mix
Selecting the optimal combination of healthcare software requires careful consideration of organizational needs, existing infrastructure, and future growth plans.
Healthcare leaders must balance immediate operational requirements with long-term strategic objectives while ensuring that chosen solutions can adapt to evolving regulations and care models.
When evaluating healthcare software options, here are some key considerations that can help you make smarter, future-proof choices:
- Integration Capabilities: Ensure new software can communicate effectively with existing systems through standard protocols like HL7, FHIR, or APIs. Isolated systems create data silos that hinder care coordination and operational efficiency.
- Scalability and Flexibility: Choose solutions that can grow with your organization. Cloud-based platforms often provide better scalability than on-premise systems, allowing you to add users and functionality without major infrastructure investments.
- User Experience and Adoption: Even the most feature-rich software fails if users resist adoption. Prioritize solutions with intuitive interfaces and comprehensive training programs. Consider involving end-users in the selection process to ensure buy-in.
- Compliance and Security: Verify that software vendors maintain current certifications for relevant regulations like HIPAA, HITRUST, or FDA requirements. Security features should include encryption, access controls, and audit trails.
- Total Cost of Ownership: Look beyond initial licensing fees to consider implementation costs, training requirements, ongoing maintenance, and potential customization needs. Factor in the efficiency gains and revenue improvements the software might deliver. Understanding custom healthcare software costs helps you make informed build-versus-buy decisions.
- Vendor Stability and Support: Evaluate vendors' track records, financial stability, and commitment to healthcare. Strong vendor support becomes critical when issues arise or regulations change.
- Customization Options: Determine whether off-the-shelf solutions meet your needs or if custom development might provide better long-term value. Custom healthcare software development can address unique workflows and requirements that generic solutions cannot accommodate.
Transform Your Healthcare Technology Strategy with Pi Tech
Healthcare software isn’t a luxury anymore. It’s the foundation of modern care delivery. As regulations evolve, patient expectations rise, and technology advances faster than ever, the real challenge is building a connected ecosystem where every system, app, and data source work together to make care safer, faster, and more human.
At Pi Tech, we don’t offer cookie-cutter solutions. We partner with healthcare organizations to design and build custom software that fits your exact needs, scales with your growth, and meets the highest standards for security and compliance.
From telemedicine platforms and predictive analytics tools to wearable integrations and advanced data pipelines, our solutions are built to handle high volumes and integrate seamlessly with your existing infrastructure.
When you work with Pi Tech, you gain get a true technology partner:
- A Senior-Level Team That Thinks Beyond Code: We don’t just follow specs. We anticipate challenges, question assumptions, and make informed decisions that move your project forward faster.
- Specless Engineering for Speed and Flexibility: Instead of waiting months for rigid requirements, we start with your goals and iterate quickly, helping you see results and value from day one.
- Proven Expertise in Regulated Industries: Every solution we build meets HIPAA, HITRUST, and FDA standards. Security and compliance are built in, not added later.
- Solutions That Deliver Real Impact: Our clients use Pi Tech-built tools to predict patient needs, improve care coordination, reduce operational costs, and unlock new revenue opportunities, all without overloading internal teams.
Whether your goal is to unify patient data, launch a digital health platform, or modernize legacy systems, Pi Tech gives you the confidence that it’ll be done right.
Ready to elevate your healthcare technology strategy? Let’s talk about how we can help you move faster, minimize risk, and turn your biggest challenges into lasting advantages.
Frequently Asked Questions
What are the 5 Most Common Types of Healthcare Software?
The five main types are Electronic Health Records (EHR) systems, practice management software, telemedicine platforms, medical imaging and diagnostic software, and healthcare analytics platforms. Each serves a specific purpose: EHRs centralize patient data, practice management tools handle scheduling and billing, telemedicine supports remote consultations, imaging software aids diagnostics, and analytics systems turn data into insights. Together, they create a connected ecosystem that improves care delivery and efficiency.
What Type of Software is Used in Hospitals and Clinics?
Hospitals and clinics use a mix of systems working in sync. Common examples include EHRs for patient records, practice management tools for scheduling and billing, and lab information systems for test results. Larger facilities add PACS for imaging, pharmacy management systems for medication control, and emergency department software for triage. Enterprise systems may also include ERP software to manage finance, HR, and supply chains. The mix depends on size, specialty, and patient volume.
How Do Different Types of Medical Software Work Together?
These systems communicate through standard protocols like HL7, FHIR, and open APIs. For instance, patient demographics entered in practice management software flow automatically to the EHR. Lab orders placed in the EHR are sent to the lab system, and results return to the provider. Imaging studies go to PACS, and analytics platforms pull data from all of these to generate reports. Smooth integration requires good planning, solid technical expertise, and continuous maintenance.
What's the Difference Between EHR and Practice Management Software?
EHRs focus on clinical care. That is, medical histories, diagnoses, medications, and lab results, while practice management systems handle the business side (scheduling, billing, and insurance claims). In short, EHRs manage the what of patient care; practice management tools manage the when and how much. Most healthcare organizations use both, tightly integrated for smooth data flow across departments.
Which Healthcare Software Type Should Small Practices Implement First?
Start with an integrated EHR and practice management system. It covers the essentials such as charting, scheduling, billing, and e-prescribing, in one platform. Once that foundation is in place, add telemedicine to reach more patients and improve convenience. Later, consider analytics or imaging tools as your data volume grows. The key is to scale step by step rather than overloading your team from day one.
How Much Does Healthcare Software Typically Cost?
Pricing varies by size and complexity. Small practice EHRs usually cost $200 to $500 per provider monthly, with setup fees between $10,000 and $50,000. Enterprise EHRs can run from $50 million to $500 million+ over several years. Practice management tools range from $100 to $400 per provider monthly, while telemedicine platforms start around $50 to $200. PACS solutions range from $50,000 to several million, and analytics systems start at around $50,000 annually. Custom development costs more upfront but can yield better ROI for complex needs.
What are the Latest Types of Health Information Technology?
Emerging technologies are transforming care delivery. AI-powered decision support now assists clinicians with diagnosis and treatment. Remote patient monitoring uses wearables to stream real-time vitals. Blockchain improves secure data sharing. Voice-enabled documentation reduces charting time. Predictive analytics spots at-risk patients before complications arise, while computer vision and natural language processing enhance imaging and data extraction. These innovations are moving quickly from pilots to mainstream healthcare use







